Expert Guidance
Access a wealth of knowledge from healthcare professionals to make informed decisions during pregnancy. We’re with you every step of the way.
Natural Remedies
Explore effective home remedies that support health and wellness throughout pregnancy. Embrace holistic approaches to care for you and your baby.




News
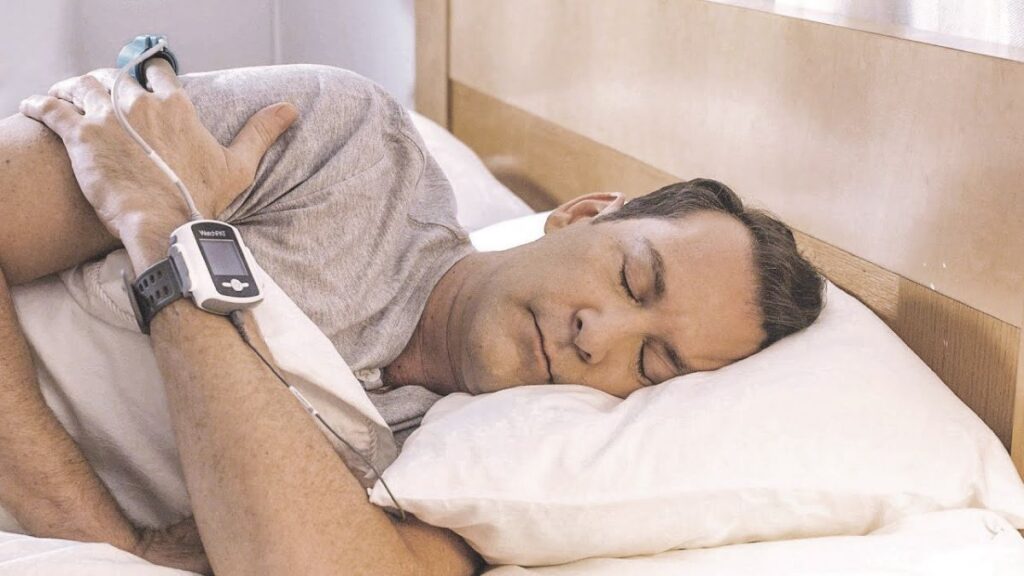
Why You Should Book a Sleep Study Adelaide Now
What Is a Sleep Study and Why Is It Important for Diagnosing Sleep Disorders? A…
Finding a Bulk-Bill Sleep Study Perth in Western Australia
What Is a Bulk-Bill Sleep Study and How Does It Work in Perth? A bulk-bill…
How Long Does Laser Eye Surgery Last? Real Results and Long-Term Studies
One of the most common—and most reasonable—questions people ask when considering laser eye surgery is:“How…
Sleep Study Adelaide: Why Early Assessment Is Essential for Better Long-Term Health
What Are Sleep Studies and How Do They Benefit Long-Term Health? A Sleep Study Adelaide…
Your Complete Guide to a Sleep Apnea Test Australia: Costs, Process and Expectations
What Is Sleep Apnea and Why Should You Get Tested for It? Sleep apnea is…
Perfect LASIK Surgery Success Stories That Will Inspire You
Introduction For many people, the thought of living without glasses or contact lenses feels like…


Our Process
How We Support Your Pregnancy Journey
What Others Say